Nutrition plays such an important role in our pregnancies and post-partum periods. Breastfeeding requires time…

Do You Know Everything You Need to Know About Your Birth Control Pill?
How much do you really know about your birth control pills? The side effects of oral contraceptive pills (OCP) are well established, yet women are often uninformed when it comes to how this widely used medication can affect our bodies. I would like to talk about the anatomy of the female genitalia and how birth control pills can affect these tissues. As you make decisions for yourself or for your daughters, you should be informed so that your decision best assesses the risk vs. benefit of the drug. I hope this blog gives you a starting point for questions to ask your healthcare provider before beginning a medication that could potentially impact your health and quality of life.
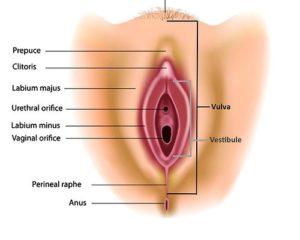
Anatomy of the Female Genitalia
Let’s start with a brief anatomy lesson. The female genitalia, namely the vulva, vestibule and vagina can be seen in the picture here.
The vulva houses the external genitalia structures (mons pubis, labia majora, labia minora, clitoris). The vulva provides protection from infection. It is different, on a cellular level, than the vestibule or vagina. In fact, these three areas develop from different cells embryologically, making them distinct for different functions. The vestibule contains several glands and the urethral opening within it, and serves the function of producing mucin, for lubrication during intercourse. Problems within the vestibule can greatly impact urination and sexual function. The vagina is a mucosal endothelial layer with folds, allowing for lengthening to accommodate a penis or delivery of a baby. Each structure responds differently to different hormones.
Many women and young girls are placed on birth control pills, not necessarily for preventing pregnancy but for varying reasons. Migraines, heavy periods, acne and mood swings are just a few. They then remain on birth control through their adult lives, until they decide they may be ready to have children. So what, right? Most everyone I know is on an oral contraceptive, they’ve been around for many years. Well, when you look at how these medications work you may change your thinking.
What is Birth Control Made Of?
OCPs are made up of synthetic hormones. By placing these fake hormones in your body, the body thinks there are enough sex hormones (estrogen, progesterone and testosterone), and it stops production from the ovaries, which halts ovulation and prevents pregnancy. Birth control pills also effect a naturally occurring protein in your body called sex hormone binding globulin (SHBG). SHBG binds testosterone and renders it inactive. When women take birth control pills, their SHBG levels are elevated. Higher SHBG levels and an already reduced production of testosterone by the ovaries leads to little to no available testosterone. Worse yet, these levels of SHBG often remain elevated even years after OCP discontinuation.
Birth Control Pills and Sexual Function
Sex hormones are important to women for many reasons. Estrogen, Progesterone and testosterone serve very important functions in the female body. Cardiovascular, bone health, sexual desire and arousal, mood, cognition and reproduction are all influenced by these hormones. When young women spend several years on birth control pills, with reduced production of sex hormones and elevated SHBG, any of these systems can be affected.
There is evidence that OCPs negatively impact female sexual function. One study of female medical students found a significant difference in sexual function measured on the Female Sexual Function Index (FSFI), between those on birth control pills and those who were not. The FSFI measures desire, arousal, pain and satisfaction with sexual intercourse. The women who were on OCPs had significantly lower scores on this measure compared to those not taking them (1) Another study by Smith et al. found that women using oral contraceptive method experienced less frequent sexual activity, arousal, pleasure, and orgasm and more difficulty with lubrication. (2)
Painful Sex and Birth Control
It is also common for women on birth control to complain of painful intercourse, also called dyspareunia. Some women may have pain in the vulva or vestibule. Other symptoms that may arise are frequency of urination or burning with urination. Recurrent urinary tract infections or yeast infections are also common among contraceptive users. A recent study showed that women who took Yasmin™ had shrinkage of their labia minora, a reduction in the diameter of the vulvar vestibule, and a reduction in clitoral blood flow as measured by ultrasound after just 3 months of taking this OCP. (3)
Just like when you enter menopause and your estrogen levels deplete, the same is happening for women on birth control pills. Decreases in the levels of these hormones cause permanent changes in the tissues and structures of the female genitalia. When these tissues are chronically irritated they become inflamed, and mimic symptoms of UTI or yeast infection. This can lead women down a long road of misdiagnosis and unnecessary treatments for conditions they don’t actually have. These concerns need to be expressed to your provider. If they discount the effects of OCPs or don’t know anything about it, it is time to find a new provider.
How Does Birth Control Effect Your Vaginal Tissues?
The evidence is out there. Many studies have shown that OCPs have a negative impact on female genitalia, particularly to the vestibule, which most impacts sexual function. A study by Johannesson et al. examined how birth control pills caused the development of microscopic structural changes in the vestibule, making these women more susceptible to tears or irritation (4). Another study showed that “healthy” women without any complaints of pain in their vulvar vestibule who are taking OCPs have a lower pain threshold than women who do not take OCPs. (5) This means their tissues have become more sensitive to touch, more easily irritated.
Yet another study looked at women who began birth control before the age of 17 and found they were 1100% more likely to have pain in their vestibule versus those who had never taken OCPs (6). In addition, Bouchard et al. found that women who do have pain in their vestibule were 960% more likely to develop vestibulodynia if they started OCPs before age 16. They also demonstrate an increased risk of vestibular pain with longer durations of OCP use (7) Another very recent study published in Sexual Medicine as a case series of 50 women who developed vestibulodynia while taking OCPs (8).
Birth Control and Women’s Health
In a society that pushes birth control, what does this all mean for women’s health issues? First off, women develop their bone health at very early ages and it depends on sex hormones. Most of our physiological function as women revolves around our menstrual cycle and these sex hormones. If we are putting young girls on OCPs at early ages, we are not only putting them at risk for sexual dysfunction as they get older, but are we also putting them at greater risk for poor bone development, heart disease, mental health issue and fertility concerns?
As a Pelvic Physical Therapist I cannot tell you how many young women I see who were put on birth control at 13, 15 and 16 years old for varying reasons, but often not because they were actually sexually active. They then have their first sexual experience either on their wedding night or not, and it is either very painful or they are unable to have it at all due to pain. The emotional trauma and inter-relational stress this causes these young women is devastating.
In 2015 an International Consensus Conference on Vulvar Pain was held to examine levels of evidence surrounding causes of vulvar pain and associated factors. During this meeting, it was decided that hormonal insufficiencies can cause vulvar pain. There are multiple references listed below, as well as some great blog articles by researchers and physicians who are experts in this topic. Please consider this before you jump to OCP’s. Consider all options with your physician and ask them questions about this research. If they shrug it off, I would consider another provider.
If you are having pain with intercourse or pain in your vulva or vestibule you should seek care from a provider who is knowledgeable about vulvar conditions. Often a pelvic physical therapist is implemental in this care, and we can also help you find the medical providers who can be a part of the team you will need to get well.
- Sarah Dominguez, PT, MSPT, CLT, WCS
This blog is here for your help. It is the opinion of a Licensed Physical Therapist. If you experience the symptoms addressed, you should seek the help of a medical professional who can diagnose and develop a treatment plan that is individualized for you. If you enjoyed this blog, check out our website at foundationalconcepts.com for more blog entries and to learn more about our specialty PT practice, Foundational Concepts. Follow us on Twitter @SarahpelvicPT or @Jenn_pelvic_PT and like us on Facebook/Foundational Concepts for updates.
References.
- https://www.guttmacher.org/united-states/contraception
- Smith NK, Jozkowski KN, Sanders SA. Hormonal contraception and female pain, orgasm and sexual pleasure. J Sex Med. 2014 Feb;11(2):462-70.
- Battaglia C, Battaglia B, Mancini F, et al. Sexual behavior and oral contraception: a pilot study. J Sex Med 2012;9:550-7.
- Johannesson U, Blomgren B, Hilliges M, Rylander E, Bohm-Starke N. The vulval vestibular mucosa-morphological effects of oral contraceptives and menstrual cycle. Br J Dermatol 2007;157:487-93.
- Bohm-Starke N, Johannesson U, Hilliges M, Rylander E, Torebjork E. Decreased mechanical pain threshold in the vestibular mucosa of women using oral contraceptives: a contributing factor in vulvar vestibulitis? J Reprod Med 2004;49:888-92.
- Bazin S, Bouchard C, Brisson J, Morin C, Meisels A, Fortier M. Vulvar vestibulitis syndrome: an exploratory case-control study. Obstet Gynecol 1994;83:47-50.
- Bouchard C, Brisson J, Fortier M, Morin C, Blanchette C. Use of oral contraceptive pills and vulvar vestibulitis: a case-control study. Am J Epidemiol 2002;156:254-61.
- Burrows LJ GA. The treatment of vestibulodynia with topical estradiol and testosterone. Sex Med 2013;1:30-3.
- http://www.nva.org/wp-content/uploads/2015/01/2015_ISSVD_ISSWSH_and_IPPS_Consensus_Terminology.2.pdf
- http://www.sophiebergeron.ca/images/publications/Pukall_2016_Vulvodynia.pdf
- American College of Obstetrics and Gynecology: http://www.sophiebergeron.ca/images/publications/Bornstein_2015_ISSVD.pdf
- http://www.pelvicpainrehab.com/female-pelvic-pain/2219/oral-contraceptive-pills-cause-vulvodynia-time-finally-end-controversy/
- http://www.pelvicpainrehab.com/female-pelvic-pain/3953/jagged-little-pill-oral-contraceptives-wreak-havoc-female-body/