Lichens...What??? I thought that grows on rocks, not my vagina. Lichen sclerosus is a skin…
Lichen Sclerosus (Like in Skler O Sus): What?
Itching “down there” is a common complaint but one that we shouldn’t ignore. When we talk to our patients about itching, many have been treated for recurrent yeast infections for years but continue to have itching. This is always a red flag that something else may be going on.
Something that we see in pelvic floor physical therapy are women with lichen sclerosus (LS) LS is a chronic inflammatory skin condition of the vulvar tissues. The symptoms that people often describe are itching or burning of the vulvar tissue, tearing sensation with vaginal intercourse, and pain with urination or bowel movements.
It is important to know the difference between the vulva and vagina. The vulva is the external female genitalia including the labia majora and minora, the clitoris and clitoral hood. The vagina is the canal from the opening of the vulva up to the uterus. The Vestibule is the “foyer” for the vaginal opening.
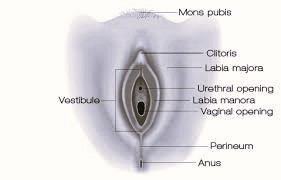
Lichen sclerosus often appears in the shape of an hourglass around the labia and vestibule (opening to the vagina), perineum (the area between the vagina and anus), and the perianal region. Some skin changes that will appear are:
- redness with cracking or tearing
- erosions that can appear white or lacey
- flattening of labia minora
- fusing of the labia minora to the labia majora
- flattening of the clitoral hood
- fusing of hood to the glans of the clitoris
It is important to see a provider who knows how to assess and treat vulvar skin conditions. Lichen sclerosus is a progressive skin disorder that will need lifelong maintenance. Untreated, there is continued inflammation that can increase the risk of vulvar cancer. Lichen sclerosus can have periods of flares and remission. Triggers for flares include increased stress, anxiety, heat, food or environmental sensitivities, and exposure to irritants like urine, scents or dyes.
The gold standard of treatment is steroid cream to decrease and manage symptoms as instructed by a qualified health care provider. This can be a Gynecologist, Uro-Gynecologist, or Dermatologist.
Pelvic floor physical therapy is an important part of decreasing symptoms. Since the skin is irritated, the pelvic floor muscles can become tight and have difficulty relaxing or elongating. This can contribute to the pain with urination, bowel movements, and intercourse. Pelvic floor PTs work closely with gynecologists, dermatologists, or primary care providers that are managing the steroid creams. Pelvic floor PTs also have more time with patients to continue education on vulvar hygiene and decreasing irritants.
It is important to have vulvar itching assessed especially if the itching continues after multiple yeast infection treatments. It is important to have a treatment plan in place with your health care provider and pelvic PT to decrease the itching and decrease pain or burning with intercourse.
If you have questions or concerns about pelvic floor PT, we offer a free, 15 minute consultation to answer any questions you may have to ensure you are in the right place for healing.