Pudendal neuralgia: pain along the pudendal nerve
Pelvic pain can be challenging to figure out. It can be embarrassing to talk about. It can effect the most personal parts of our lives including sexual function, bowel and bladder symptoms. This pain can become a wedge in relationships with partners. Often, providers aren’t sure what’s going on either or who to refer to for the best treatment, which increases the worry about what is wrong. Nerve pain is one of the most challenging contributors to pelvic pain.
Nerves can become irritated along the entire length of the nerve, from the nerve root where the nerve comes off the spinal cord, or along the peripheral nerve path to the endings. Why do they become irritate? Anywhere that the nerve makes a sharp turn, sits along a bone, or where the nerve can be compressed by tissues can decrease the blood flow to the nerve. Also, tasks or movements that cause tension in the nerve like deep squatting, straining as in childbirth, or other repetitive stressful movements can cause a traction type injury to nerves.
The pudendal nerve is a nerve that comes off the sacral portion of the spinal cord and innervates the anal opening, perineal body, and the tip of penis or clitoris. The nerve travels from the front side of the sacrum and dives around the pelvic opening. There it threads between the sacrospinous and sacrotuberous ligaments through an area called Alcock’s canal. From there it travels the inside of the ischial tuberosity (sits bones) where it branches to the anal, perineal, and clitoral/penile branches.
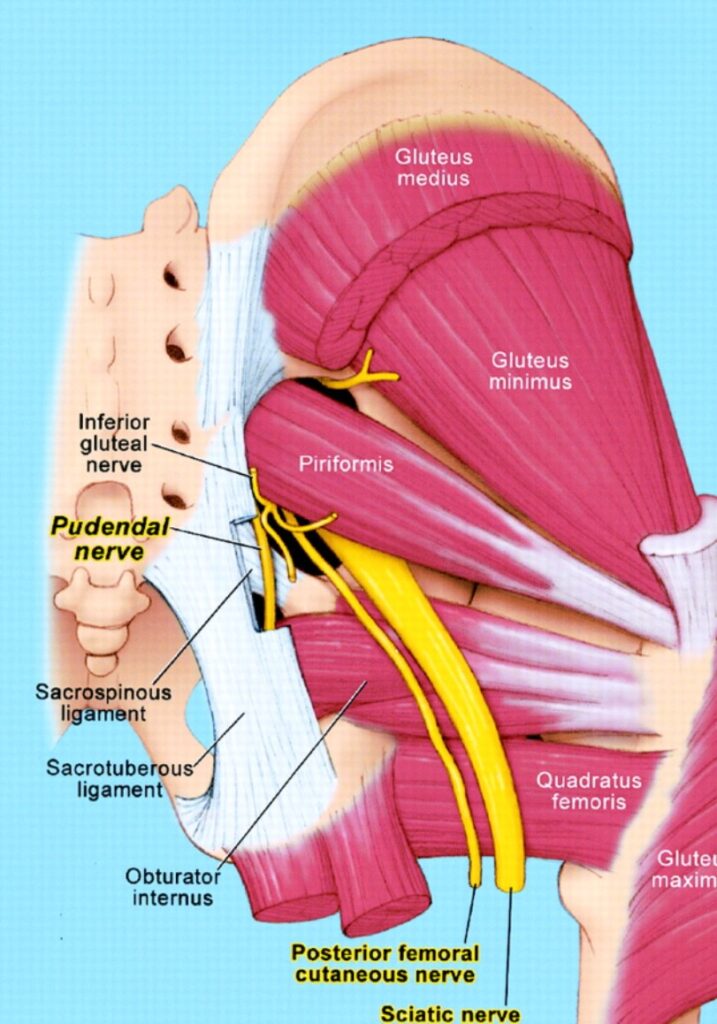
This nerve can become irritated with prolonged sitting, with tissue changes during and after menopause, with prolonged pushing during delivery, or repetitive staining with lifting or chronic constipation. If muscles in the pelvis have increased tone or decreased fascial mobility, the tissue can increase pressure on the nerve or decreased blood flow to the nerve. This pressure or traction on the nerve can cause pain, burning, tingling, muscle guarding and tension, or weakness.
This can cause symptoms like:
- Burning, tingling or sharp pain in the perineum (area from the anus to the clitoris or tip of the penis)
- needing to pee more often
- pain when peeing or pooing
- constipation
- a feeling of swelling or fullness in your anus or vagina
- difficulty getting an erection
- difficulty reaching orgasm
- pain when having sex
Pelvic floor physical therapy is an important provider if you are experiencing or suspect that you are experiencing pudendal nerve pain. It is important that the PT program include hip and pelvic floor mobility, muscle elongation, soft tissue manual release along the entire length of the nerve and movement. Pelvic floor PTs are excellent resources in referring patients to pain management, urogynecology, urology, or gynecology providers who are comfortable treating pudendal nerve pain.
Any nerve pain can require a team of providers to figure out the cause of the pain, manage medications, assist in the psychological effects of pain, and work on a mobility and stability of the nerve and surrounding tissues.
At Foundational Concepts we specialize in all things pelvic floor! We offer a free, 15 minute consultation to answer your questions and help you feel at ease in finding a therapist who can help you heal.

