When you look at how to manage prolapse, one of the first things that you…
What is Intra-abdominal pressure and how does it contribute to Pelvic Organ Prolapse?
Increased intra-abdominal pressure is a large contributor to pelvic organ prolapse and to worsening symptoms. When you see a pelvic floor physical therapist for pelvic organ prolapse, one of the first things we will look at is how well you manage the pressure in the abdominal wall.
The way that I describe this to my patients, is to talk about a pop can. If you have a pop can sitting on a shelf, the pressure on the inside pressure meets the pressure on the outside. The sides of the pop can are firm, and the pressure is equal. If you shake up the pop can or put the can in the freezer, the pressure in the can increases and the ends may push out. Now the pressure inside the can increases and is higher than the outside of the can. Your abdominal cavity is similar. Your muscles, fascia and ligaments support the walls of the abdominal cavity. Good muscle coordination keeps the pressure mechanics in check. If they are injured, or become dysfunctional, this can contribute to pain, constipation, or difficulty emptying your bladder. On the reverse side, if you pop the tab of the can, the pressure on the outside now is higher than the inside pressure and the sides of the can become soft. Similarly in your body, when one muscle is weakened, this can contribute to urinary leaking, decreased core strength, prolapse and pelvic instability, and back or hip pain.
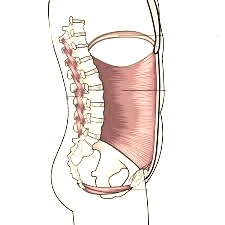
Abdominal muscles, Diaphragm, spinal muscles and pelvic floor muscles make up the cannister that supports the abdominal cavity.
With a prolapse, our abdominal pressure is like the open pop can. Due to the “leak in the system” it can be difficult for the pelvic floor muscles, diaphragm, and abdominal wall to work together. If you cough or sneeze, the abdominal wall and pelvic floor are not able to resist the heavy downward pressure from the diaphragm causing urinary leaking.
So how do you manage intra-abdominal pressure?
- Good coordination of the diaphragm, abdominal wall, and pelvic floor muscles. When you breathe in, the diaphragm descends, and the pelvic floor should lengthen. When you breathe out, the diaphragm rises back up and the pelvic floor shortens.
- Good lifting mechanics. If you hold your breath when you lift, there is more downward pressure on your pelvic floor and abdominal contents. This will worsen the prolapse over time. If you have to hold your breath to lift something, please ask for help to lighten the load.
- Prevent constipation. If you are straining to have a bowel movement, there is more downward pressure on the pelvic floor every time that you poop. It is important to manage constipation either with diet, water, stool softeners, and pelvic floor PT for improved toileting techniques.
- Manage coughs. If you have a chronic cough, it is important to try to manage it. Coughing increases abdominal pressure with increased downward pressure and increased stress on the pelvic floor and pelvic fascial tissues.
Pelvic floor PT plays an important role in developing a plan for helping to manage abdominal pressure with different daily tasks or gym activities. We can assess your current ability to coordinate these muscles, and teach you how to manage your pressure mechanics, for different tasks, how to safely return to the gym and whether or not you need to seek help from a surgeon for your prolapse. Many prolapse can be managed conservatively with physical therapy! If you have a prolapse, please reach out to your pelvic floor PT to develop your plan. We offer a free, 15 minute phone consultation to make sure you are in the right place for healing!



